On March 31st, Sonoma County’s chief public health officer Dr. Sundari Mase extended the county wide shelter-in-place order through May 3rd. The new order both keeps in place and expands previous restrictions. All state, local and county parks in Sonoma County will continue to remain closed. While most residents are sympathetic to the order, some have begun to question whether the full park closure continues to be necessary.
The original stay at home order enacted on March 17th left parks open, listing them as essential to mental and physical health–which they clearly are. Then on March 24th, after a weekend which Rohish Lal, Sonoma County Public Health’s communication officer, characterized as busier than peak summer weekends, the decision was made to close all parks and public lands in Sonoma County. “Vast numbers of people were using the parks,” Mr. Lal said. “We have it in the community and we’ve taken drastic steps. If there is no congregation of people, it can’t spread.”
While deemed necessary by public health experts, the closures of public recreation spaces are especially unfortunate given that in initial stay-at-home orders, both at local and national levels, they were listed as essential to mental and physical health. This is especially true for members of our community without private yards and property, or who live in smaller spaces. The Sonoma Independent published an article, now removed after the revised local order, informing the public that parks were still open because of their unique benefits for physical and mental health.
Mental health is a major and often unaddressed issue that is affecting millions during this crisis. A recent article in the Washington Post discussed how many Americans are suffering from increased anxiety and other mental health problems. A poll cited showed that 45% of respondents reported that covid-19 has had a negative effect on their mental health, with almost 20% saying it had a major impact.
Dr. Carrie Aigner Ph.D., a psychology professor who teaches health psychology at Humboldt State University, said regarding the relationship between time in nature and mental health, “There’s actually quite a bit of research looking at the physical and mental health effects of being in nature. Consistently, the research demonstrates that exposure to nature and green spaces help us in numerous ways including decreasing blood pressure, lowering stress, improving mood and enhancing cognitive functioning.”
Even though residents of Sonoma County cannot at this time use the public parks that our taxes support for their health benefits, Dr. Aigner offered some alternatives to receive this benefit from within our own homes. “What’s interesting about this research is that it suggests that even viewing green space from your window (or having a houseplant) can be beneficial; this has implications for people who might not be able to easily go outside, including those with mobility limitations.”
The Sonoma County shelter in place order is set to expire on May 3rd. When asked at a press conference on April 8 when the order might be lifted, Sundari Mase, the County’s top health official, said that this depends on “what that curve looks like for our outbreak.”
Mase said public health workers will be closely tracking the decline of the outbreak, both in terms of fewer hospitalizations and cases over a period of time. “It doesn’t mean shelter-in-place has to be in for a very long time,” she replied. “What it means is that we need to look at the impact of these other measures that we’re putting in place.”
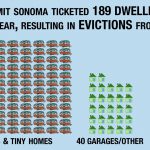
As of now it seems that the county’s early shelter in place order has been highly effective in limiting the transmission of the virus, and that all of the more dire scenarios once predicted have been avoided. With 500,000 residents, Sonoma County has reported fewer than people with the virus and only one death. According to County Health Department reports, only 21 of these have required hospitalization–a number that has, thankfully and importantly, barely increased during the past ten days.
It is impossible to gauge whether closing public access to public parks was necessary or whether it was an overabundance of caution. The Sonoma Independent asked Bert Whitaker, the Head of the county Parks Department, in writing whether they had evidence of virus transmission linked to outdoor park interaction, and he responded by sending the previously released county press release on the closure.
On April 10th, Mendocino officials revised their shelter-in-place order to re-open parks in a limited capacity. The order allows residents to hike, walk, or bike in parks within walking or biking distance from their home. Social distancing guidelines are still required within parks and residents are encouraged to use face coverings. With one fifth the population of Sonoma county, Mendocino has only four known coronavirus cases.
Rohish Lal of the Sonoma County Health Department said that Sonoma county still hoped to be able to lift the park closure order on May 3.
When asked if there was any criteria in place that could allow some parks to open early, he said that the park closure was at this time tied to the countywide order. He noted that regardless of the county’s decision, the governor’s orders would supersede anything done at the county level. Gavin Newsom meanwhile said that he still expects California’s peak to come in mid May and has discussed extending the stay-at-home until June. He noted that models and a lower than expected number of deaths were showing that the order was effective.
It cannot be overstated that since covid-19 is a novel virus, much is not known. Because of this it is hard for experts and officials to chart a path forward. There is broad agreement that the shelter-in-place orders currently in place are necessary and working, but less agreement on how to end the lockdowns without causing another serious outbreak.
In an interview with the Washington Post, The Chief Health Officer of Santa Clara County, Dr. Sara Cody, discussed what the path forward away from the current strict controls could look like. While she acknowledged that there was much uncertainty, she expressed optimism that once the number of cases falls to a low enough level, the stay-at-home orders will be able to be at least partially lifted. Once this happens, California can hopefully go back to a containment strategy, similar to what was done in places like Singapore.
Once testing capacity is increased and an antibody test is developed to show whether a person has immunity after being infected in the past, it will be much easier to monitor the disease and contain clusters of cases. Most likely during this time there will still be some limits on large gatherings, but society can begin to function again with some level of normalcy.
This containment phase will probably need to go on until a vaccine is developed. Most experts agree that if an effective vaccine can be developed, and there are promising signs that it will be, then enough of the population can be vaccinated to produce herd immunity. Coronavirus may become endemic in the human population, but because of this herd immunity its spread will be limited and its pandemic potential eliminated. Dr. Fauci and other experts believe a vaccine is the only way to prevent a future pandemic once the current one is brought under control. The timeline for an effective coronavirus vaccine has been put at twelve to eighteen months.
While this is truly a trying time and a unique, unprecedented moment in modern history, there is light at the end of the tunnel. In the meantime, Dr. Aigner of H.S.U. had this advice for those of us who are missing parks and sunshine, “I think we all need to focus first and foremost on keeping ourselves and those around us safe. Social distancing is the best way to do that. That being said, you can find ways to be outside that don’t violate social distancing rules. Research tells us that even sitting outside in your lawn, balcony, or front step can help to improve mood and well-being. I think we all have to get creative to find ways of getting outdoors while staying safe.”
How is the disease transmitted?
While closing parks and public space is in line with what other regional jurisdictions have done, the Sonoma Independent sought to compile the most up to date information on how coronavirus spreads, what mitigation actions have taken place around the world, and what strategies seem to be working. With this information in hand, we hope that our readers will be able to better judge and understand the restrictions put in place on 97% of the people in the U.S. and over a third of the global population.
SARS-Cov-2, the virus that causes covid-19, is a novel virus. This means that human beings have not been previously exposed to it. Various types of coronaviruses are not uncommon, the common cold, along with SARS-1 and MERS, are also coronaviruses, but SARS-Cov-2 is new. It made the jump to humans from an animal, perhaps a bat or pangolin. Because of this novelty humans have no immunity to the disease it causes, covid-19.
As epidemiologists and political leaders across the globe struggle to stem the spread of the virus, it is crucial to determine the specific ways in which it is most likely to transmit from person to person. Unfortunately, since the virus has only been known since late December, data from which to draw conclusions is limited. While much has been learned already, scientists and medical professionals continue to refine what we know about the virus on a near daily basis.
In the first weeks of the pandemic the WHO and CDC recommended frequent hand washing, covering one’s face when coughing (but not wearing a mask unless sick or a health worker), isolation of individuals showing symptoms, and social distancing between individuals of 6 feet.
This number was based on the belief that virus particles are exhaled in large water droplets that travel from three to five feet before falling to nearby surfaces. Transmission was thought to occur either when individuals were in very close contact with an infected person, by breathing in expelled large droplets, or by touching a surface that the virus was on, then touching either their mouth, nose, or eyes. This is still considered to be the most likely way that the virus is transmitted.
Recent research however has cast doubt on whether the virus can only be transmitted by large droplets. These findings suggest that it may also be transmitted in the much smaller, aerosolized particles exhaled during normal breathing. Aerosolized particles may hang in the air for hours, possibly passing into ventilation systems to be spread throughout buildings. Under certain conditions, such as when a person coughs or sneezes, particle clouds can spread as far as 26 feet. These findings are far from conclusive, but the possibility that coronavirus can pass between individuals who are simply talking or breathing, and that 6 feet may not be enough, could explain why the virus has spread so rapidly.
In addition to possible spread by bioaerosols, more and more research has reinforced the idea that the disease can transmit when individuals are experiencing no symptoms. Not only can the virus pass from person to person before there is any sign of infection, but this may be the time that the virus is the most communicable.
This asymptomatic transmission is especially troubling from a public health perspective. A study from China showed that viral loads were the highest at the initial symptom onset. Others studies have also shown that people are most capable of transmitting the virus while they are still presymptomatic. Further adding to the difficulties in containing the virus, testing in Iceland suggests that many people may contract the disease and remain asymptomatic. 50% of those who tested positive for coronavirus had no symptoms at the time of testing.
The increasing severity of the pandemic, evidence of asymptomatic transmission, and the possibility of spread by bioaerosols has led the CDC and WHO to change their advice and now recommend that persons wear masks while in public. This abrupt change in guidelines shows how difficult it is for even those in the highest positions of knowledge and authority to respond to a disease that has little precedent and of which much is still unknown. While the global response to the coronavirus pandemic remains fluid, it is possible to evaluate some of various approaches that countries around the world have taken to contain the virus’s spread.
What have other countries done?
“Flatten the curve” has gone from being obscure epidemiological jargon to a household saying. While this is the goal in every country covid-19 has touched, jurisdictions have taken a variety of sometimes similar and sometimes diverging approaches to mitigate the crisis. While it is still early, weeks and in some cases months have passed since the virus’s outbreak in each location. Looking at what other governments have done, and what has worked and hasn’t, can be a good measure with which to judge actions taken locally, as well as on the federal level in the United States.
China was where the pandemic started, where it has had the longest to run its course, and was the first country to drastically relax its mitigation strategies. Decried by many in the United States as using “draconian measures” it has in many ways been the most successful in stopping the disease. Out of a country of over a billion, the country has reported a relatively low death toll of around 3,300 as of April 7th. This is a per capita mortality rate 20 times lower than the death rate in the United States. The WHO congratulated China’s response, calling it a “unique and unprecedented public health response [that] reversed the escalating cases”.
After first failing to recognize that they were facing an outbreak of a novel respiratory pathogen, China took fast and decisive action. In an interview with Science Magazine, Chinese CDC director George Gao discussed the measures in China and what was effective. Gao said that local and national cooperation was key in getting the outbreak under control, he also cautioned that western nation’s failure to mandate mask wearing was a mistake and risked presymptomatic transmission of the disease.
China used strict measures such as in-country travel bans, strict quarantines, and temperature checkpoints in stores, highways, and public places. If someone tested positive for covid-19, they were moved to massive isolation facilities away from their family. Gao said that these strict measures were key in stopping covid-19’s spread. China also continues to track individual’s movements via cell phone data and assigns them to various risk categories, which then determine the degree to which their movement is restricted, for instance whether they are allowed to enter public buildings.
A Nature article discussing which strategies were the most effective suggests that travel restrictions bought the world more time to prepare, but did not significantly stop the disease’s spread within the country. Extreme and early social isolation appears to have had the most effect on stopping transmission, but where China especially deserves credit is its successful case tracking programs and decisive top down response. China sent 40,000 healthcare workers, many of them volunteers, to the Wuhan epicenter. This allowed health officials to assign teams of five or more epidemiologists to each new case, sometimes tracing and testing a hundred contacts the infected person may have interacted with. This massive scale of tracing, testing, and isolation seems to have been the key factor that prevented China’s outbreak from taking the turn it has in the U.S.
Singapore, Taiwan, and Hong Kong are three countries that are often discussed as being public health paragons for their success in preventing large scale outbreaks even though they are both geographically close to and deeply connected to China. Singapore, like China, is a state capable of taking strict authoritarian actions. Hong Kong and Taiwan however are both democracies. What all three countries have in common is a shared experience with the 2003 SARS epidemic.
SARS shaped these countries policy response and their culture. Immediate national action was taken by the state and the public was ready for and understanding of the sacrifices they would need to make to prevent tragedy. Singapore has one of the best disease surveillance programs of any country in the world. While the one party city-state has implemented strict quarantine measures with hefty fines for violators, they have also exemplified effective and transparent crisis communication, and have supported individuals financially and medically throughout their quarantines.
Using this aggressive surveillance, testing, and isolation strategy, Singapore managed to keep cases low while leaving most businesses, schools, and public life open. This may be changing however as a second wave of infection appears to be taking place in the country. The authorities have now urged citizens to only go outside for essential needs, have closed many businesses, and are limiting the size of gatherings.
Hong Kong and Taiwan, both democracies, also stand out for their successful tracing and testing programs. In addition to these programs, both countries put in place strict social distancing measures including school and business closures. In Hong Kong, recently wracked by protests against the government, the public has stood behind public health official’s decisions.
In Taiwan, the public has supported policies that in China have been labeled draconian. While Taiwan’s stay-at-home orders were not as stringent as China’s, the country implemented a cell phone tracking system to make sure that covid positive individuals ordered to quarantine did so. The app is not optional and alerts police if a quarantined person leaves their home. Health officials also call twice a day to make sure that the person has not left the house without their phone.
Another commonality between the three small countries is that they all have universal health care programs. Sadly, it may be too late for the U.S. to take many immediate cue’s from these countries’ success, which was so heavily based on surveillance and early detection, tracing, and isolation.
A few countries with coronavirus cases that have resisted widespread lockdown orders are now taking action. Japan kept much of the country open, relying on testing and tracing outbreak clusters, but in recent days has seen a major growth in cases. The government has now declared a state of emergency and urged individuals and businesses to close. The Japanese state lacks legal authority to enforce stringent lockdown, but is hoping that people will listen.
Out of the European countries, Sweden has, controversially, taken a more narrowly focused approach, banning large gathering, quarantining seniors, but allowing its parks to remain open. Yet the spread of the virus, and the death toll there, is less than in surrounding nations with similar populations and far stricter lockdown orders. . For countries like Brazil, where national leaders have not instituted widespread lockdown orders, the next few weeks will be a test of how successful the measures, or lack thereof, are in preventing catastrophic loss of life.
Italy was the first European country to have an outbreak and it was forced to enact some of the strictest measures to combat the virus. The loss of life there is nearing 19,000 as of April 10th, but there is now clear evidence that their mitigation efforts are successfully flattening the curve. The percent increase of new cases continues to fall and the death rate, while still high, has apparently stabilized. Italian government officials are beginning to discuss ways to open the country without starting another outbreak, but officials warn that though there is light at the end of the tunnel, it is still a long road ahead. Lorenzo Casani, the health director of a clinic in Lombardy, told Time Magazine “Draconian measures are still needed. It’s the only way to avoid a catastrophe.”
Social isolation measures are working in the U.S which may allow easing of some of them soon
Due to its lack of a coordinated national response, the U.S. will likely serve as a case study in evaluating the efficacy of more and less stringent lock down orders. Already data suggests that the jurisdictions which were first in the nation to put in place strict stay-at-home orders have suffered the least loss of life. Areas that waited longer, or put in place less strict or optional orders, have fared worse.
The San Francisco Bay Area counties led the nation in enacting the first large scale stay-at-home orders on March 16th, followed by a statewide order on the 19th. New York waited five days after California and has witnessed an explosion in case numbers and deaths. Bay Area hospitals have remained under capacity and have kept death rates low. While New York is a much larger and denser metropolitan area, the Boston metropolitan area shares many similarities with the Bay Area. Boston waited until March 24th and currently has approximately three times the cases per capita as the Bay Area. Case numbers and deaths in Massachusetts continue to grow at an alarming rate.
Data from other states also point to the effectiveness of early and complete stay-at-home orders. Ohio acted very early, with hospital officials putting plans into effect as early as February. The state’s Republican governor was one of the first in the nation to cancel school and large commercial events, even at the cost of millions to the state. Ohio now has comparatively one of the lowest levels of infection and death in the nation.
Washington state also took early action and even with one of the initial outbreaks in the country, has had good success in keeping numbers low. It’s too early to know for sure, and California public health officials still expect a surge, but one thing is clear; early stay-at-home orders slowed the spread of the disease, preventing hospitals from being overwhelmed, and gave California’s institutions valuable time to prepare and take action.
Everyone wants life to go back to how it was before the coronavirus. And shelter-in place orders can’t last forever.
The good news is that we shouldn’t have to wait the full year or eighteen months for a vaccine before the strictest measures are lifted. In Sonoma County there are already clear signs of hope “The good news is this — we are not finding a lot of community transmission any longer,” Dr. Sundari Mase, Sonoma County’s public health officer said. County fairs and music festivals will probably still be cancelled this summer, but if current trends continue, there’a a good chance we’ll have access to our parks.